This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Radhesh Mahankali.
66 year old male maggam worker or weaver by occupation resident of Narketpally came with chief complaints of:
Fever since 10 days.
Pain in the abdomen.
Shortness of breaths from 10 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 1 month ago then in the month of may he developed fever for 5 days which was insidious in onset intermittent in nature, aggravated on food intake and aggravated during night, temporarily releived on medication.
Then he complained of fever which was continuous and high grade associated with chills and rigors since 10 days.
He also had C/o loose stools 20 days back for 5 days, 3 episodes per day, small volume, watery in consistency.
Not associated with constipation, blood in stools, foul smell of stools, presence of worms in stools.
He complained of pain abdomen in the right hypochondrium since 20 days from (25th of may) which was insidious in onset, gradually progressive, intermittent, pricking type aggravated during nights and
before defecation and releived on passing stools and the pain was non radiating.
Patient also developed SOB since 5 days on walking up a slope or on hurrying (MMRC GRADE 1) since 20 days and it progressed to the current state where he has to stop for breath in between his work (MMRC GRADE 2) relieved on rest. SOB not associated w cough, chest pain, chest tightness, hemoptysis, PND, wheeze and orthopnea.
PAST HISTORY:
No similar complaints in the past.
N/K/C/O HTN, asthma, epilepsy, TB, CVD, CVA and Thyroid disorders.
FAMILY HISTORY:
Not significant.
PERSONAL HISTORY:
Sleep-adequate
Appetite- normal
Addictions-
Alcoholic since 40 years: 90ml of whiskey per day everyday. Last consumption was 1 month ago.
Chronic smoker since 20 years: smokes 1 pack of beedis per day (each pack contains 20 beedis).
Bowel: regular
Bladder: regular
Allergies: no known allergies.
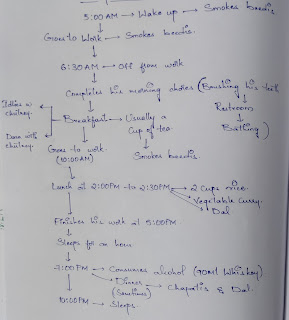
DAILY ROUTINE:
GENERAL EXAMINATION:
Patient was conscious coherent and cooperative well oriented to time place and person, moderately built and nourished.
CLUBBING- PRESENT
No pallor, icterus, cyanosis, lymphadenopathy, edema


VITALS:
Bp:120/80 mmhg
Pulse rate: 80 bpm
RR: 21 cycles per min
Temp: Afebrile.
SYSTEMIC EXAMINTATION:
CVS: S1, S2 heard, No murmurs heard
RS: BAE +
Crepitations were heard in infra axillary region.
Ronchi are heard in infra axillary area.
CNS: No focal neurological defect
Per Abdomen :
INSPECTION:
Shape of abdomen: scaphoid
Umbilicus : inverted
Guarding of abdomen present.
No visible swellings, scars, sinuses ,engorged veins, no visible peristalsis or pulsations.
A patch is present over the right lumbar region.
No local rise of temperature.
Tenderness is present in epigastric region.
Liver is palpable, lower border is felt.
Spleen not palpable, no spleenomegaly.
PERCUSSION:
bowel resonance heard.
AUSCULTATION: normal bowel sounds are heard.
INVESTIGATIONS:
BLEEDING AND CLOTTING TIME:
APTT
BLOOD GROUPING
PROTHROMBIN TIME
CUE
HEMOGRAM
BLOOD LACTATE
ECG
USG:
PROVISIONAL DIAGNOSIS:
LIVER ABSCESS
TREATMENT:
Percutaneous drainage under LA
10% NS@ 50ml/hr
Inj Magnex Forte(Sulbactum+Cefoperazone) 1.5mg/IV/BD.
Inj metrogyl(Metronidazole)500mg iv/TID
Pan 40mg BD
Inj paracetamol 1g/iv/TID
Tablets: MultiVitamin OD
Vitamin C/OD
Vitamin K 10mg/IM STAT.
















Comments
Post a Comment