50 YEAR OLD MALE WITH ABDOMINAL DISTENTION AND ABDOMINAL PAIN
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
Patient was apparently asymptomatic 8 days back then he noticed abdominal distention which was diffuse associated with abdominal pain which was squeezing type, aggravated with food intake, not associated with vomitings, loose stools ,fever.
Complaints of bilateral pedal edema which is pitting type gradually progressive , extending from ankle to knee joint.
Complaints of decreased urine output and yellowish discolouration of urine since 5 days which is not associated with fever, chills and burning miturition and frothing of urine.
No history of chest pain , palpitations , excessive sweating.
Complaints of shortness of breath with grade II which is decreased in supine position.
No history of hematemisis , melena.
PAST HISTORY:
History of dengue 3 years ago for which he was hospitalized for 15 days.
History of jaundice 2 years ago for which he was transfusions 2 PRBC'S.
No similar complaints in the past.
no history asthma, epilepsy, thyroid disorders,TB.
No history of previous surgeries.
FAMILY HISTORY : No significant family history.
PERSONAL HISTORY
DIET : Mixed
APPETITE: Decreased
BOWEL MOVEMENTS: Normal
Bladder movements: Decreased urine output since 5 days.
SLEEP : Adequate.
ADDICTIONS : Alcoholic since 12 years, he used to drink 180 ml of whiskey twice a week but, from last 6 years he began drinking 180 ml of whiskey daily, but stopped drinking 15 days ago. No history of smoking.
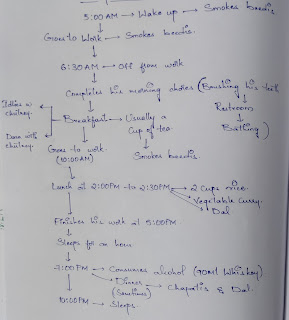
DAILY ROUTINE :
He is a government servant, field worker in revenue department who wakes up at 5 am completes his daily routine and goes to work but, most of the times he skips his breakfast. Eats lunch in between 2 - 4 pm because of his busy schedule and goes to bar at 6 pm to drink alcohol daily ( whiskey 180 ml ) and then goes home and eats dinner at 8pm and sleeps by 10 pm.
GENERAL EXAMINATION
Patient was conscious, coherent and cooperative well oriented with time place and person.
Moderately build and moderately nourished.
Pallor : Present
Icterus: Absent
clubbing: Absent
cyanosis: Absent
Lymphadenopathy: Absent
Edema : Present.
VITALS:
On 4/1/23
Temp: afebrile
BP: 110/70 mm hg supine position
Pulse: 82bpm
RR: 18cpm.
On 3/1/23
Temp: afebrile
BP : 110/70 mmHg supine position
Pulse : 92 bpm
RR : 20cpm
Grbs : 101 mg /dl
On 2/1/23
Temp : afebrile
BP : 110/90 mmHg
Pulse : 90 bpm
RR : 22cpm
Spo2 : 98%
SYSTEMIC EXAMINATION:
PER ABDOMEN :
On Inspection :
Abdomen is distended
Visible veins are seen
Umbilicus : flat
Flanks are full
Palpation :
No local rise in temperature.
Abdomen is tense.
Percussion - dull note
Auscultation:
Bowel sounds -decreased
RESPIRATORY SYSTEM :
On inspection :
Shape of chest is normal
Looks like symmetrically expanding
No scars and sinuses
Trachea is central
On palpation :
no local raise of temperature or tenderness.
All inspectory findings were confirmed.
On percussion:
Purcussion note is same on both sides.
On auscultation :
Normal vescicular breath sounds are heard.
CVS :
S1, S2 heard, Apex beat felt at 5th intercoastal space lateral to mid clavicular line, no murmurs.
CNS EXAMINATION:
HIGHER MENTAL FUNCTIONS:
Conscious, coherent, cooperative
Appearence and behaviour:
Emotionally stable
Recent,immediate, remote memory intact
Speech: comprehension normal, fluency normal
CRANIAL NERVE:
All cranial nerves functions intact.
INVESTIGATIONS:
Diagnosis: Pancreatitis secondary to alcohol intake, decompensated liver disease.
Treatment:
Ascitic tap was done but no fluid was drained.
Fluid restriction less than 1.5 L /day.
Salt restriction less than 2g/day.
Inj Lasix 40mg IV BD.
Syp lactulose 30ml PO.
Inj Monocef.
TAB Aldactone 50 mg PO OD.



















Comments
Post a Comment