50 year old male with SOB since 12 days
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
A 50 year old male vegetable vender by occupation came to GM OPD with chief complaints of:
Shortness of breath since 12 days
HOPI:
Patient was apparently asymptomatic 3 months back, then he developed SOB [Grade IV(NYHA) : SOB even on rest and minimum physical activity].
The patient had complains of SOB with severe physical activity(grade II) 3-4 years ago, which progressed to current state.
H/o decreased urine output.
H/o orthopnea, paroxysmal nocturnal dyspnea.
H/o pedal edema [present below the knee and of pitting type].
H/o cough since 12days(non productive).
No h/o palpitations, chest pain, sweating, fever, cold, headache, myalgia .
PAST HISTORY:
The patient got admitted for similar complaints 3 months ago (january) got treated and discharged.
K/c/o Heart failure with CKD.
K/c/o HTN since 3 months for which he is using (Tab.HYDRALAZINE 12.5MG PO/OD)
N/k/c/o DM, Asthma, TB, epilepsy,etc
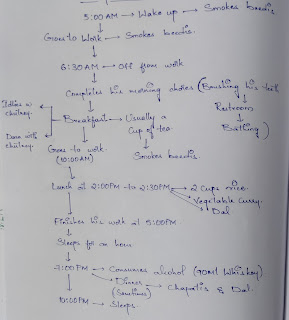
PERSONAL HISTORY:
Diet: mixed.
Appetite: decreased since 12 days.
Sleep: disturbed due to SOB.
Bladder: Decreased since 12 days with burning micturition.
Bowel: Normal
Addictions:
1) Alcoholic since 10 years( drinks half a bottle per day everyday). Last consumption was 15 days back.
2) Tobacco chewing(khaini) since 10 years(1-2 packets per day every day).
Allergies: No known allergies.
FAMILY HISTORY:
Not significant.
Patient is conscious, coherent and cooperative, well oriented to time place and person.
No pallor.
No icterus.
No cyanosis.
No lymphadenopathy.
Clubbing present.
Pedal edema present [below the knee and of pitting type].
CVS EXAMINATION:
RESPIRATORY SYSTEM EXAMINATION:
Normal vescicular breath sounds are heard.
P/A: SOFT AND NON TENDER.
CNS: NO FOCAL NEUROLOGICAL DEFICITS.
INVESTIGATIONS:
1.FLUID RESTRICTION <1LT/DAY
2.SALT RESTRICTION <2GM/DAY
3.INJ.LASIX 60MG IV/BD
4.INJ.THIAMINE 200MG/IV/TID (in 100ml NS)
5.TAB.METAPROLOL 25MG PO/OD
6.TAB.ECOSPORIN AV 75(10)/PO/HS
7.T.NODOSIS 500MG PO/BD
8.CAP.BIO D3 PO/ONCE WEEKLY
9.PROTEIN RICH DIET 2EGG WHITES/DAY
FOLLOW UP: [28/03/2023]
grade II B/L pitting type pedal edema
SOB decreased
Pt is c/c/c
Temp - 98.6°F
Bp - 120/80mmhg
Pr - 72bpm
RR - 20cpm
SpO2- 98% @ RA
GRBS:106mg/dl
CVS - S1 S2 heard , no murmurs
JVP elevated
Rs -Rt IA Crepts present, decreased air entry on rt IA region
P/A: Soft,non tender
CNS - HMF+,NFND
T/T (28/03/2023):
1. FLUID RESTRICTION <1LT/DAY
2.SALT RESTRICTION <2GM/DAY
3.INJ.LASIX 60MG IV/BD
4.TAB.BENFOTHIAMINE 200 MG PO/BD
5.TAB.METAPROLOL 25MG PO/OD
6.TAB.ECOSPORIN AV 75(10)/PO/HS
7.TAB.CINOD 10MG PO/OD
8.CAP.BIO D3 PO/ONCE WEEKLY
9.TAB.NODOSIS 500 MG/PO/BD
10.PROTEIN RICH DIET 2EGG WHITES/DAY
.
.








Comments
Post a Comment