This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Radhesh Mahankali.
43 year old male came to general medicine OPD chief complaints of :
pain in the obdomen since 3 days.
vomitings since 2 days.
HOPI:
Patient was apparently a symptomatic 2 days ago then he developed pain abdomen in the epigastric region which was sudden and onset gradually progressing, pain is aggravated on eating food and in supine position and relieved on bending forward and on empty stomach.
History of vomiting 2 days ago three episodes after eating food the vomiting was non projectile the vomit contained food particles, it was not bilious in nature and was not blood tinged.
History of itchy skin lesions over left foot since 10 years which initially started as papule for which he used an unknown topical medication.
No abdominal distension, flanks are normal, no loose stools, no history of fever, shortness of breath, No chest pain, no orthopnea, no paroxysmal nocturnal dyspnea, no night sweats, no chest tightness, no palpitations, no cough, no fever, no myalgia, no acid reflux, no syncope, no hemoptysis, no decreased urine output.
PAST HISTORY:
Similar complaints in the past 1year ago for which he was treated here and discharged.
N/k/c/o DM, Asthma, HTN, epilepsy, TB, CVD, etc.
PERSONAL HISTORY:
Diet: mixed.
Appetite: Normal.
Sleep: Adequate
Bladder: Normal
Bowel: Constipation since 2-3 days.(3 episodes of stools in 2-3 days).
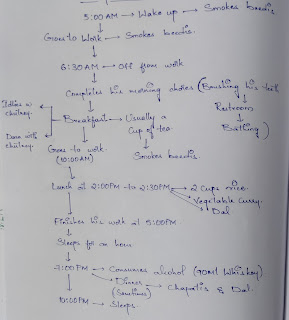
Addictions: Alcoholic: Patient is an alcoholic and 10 years started drinking Toddy 100 ml per day due to body pains from his occupation. He then shifted to drinking whisky quarter a day occationally 2 quarters a day 5 to 6 years ago His last episode of alcohol binge was 4 days ago.
FAMILY HISTORY:
Not significant.
VITALS:
Temperature: Afebrile.
PR: 76bpm.
RR: 19cpm.
BP: 130/90 mm hg.
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative, well oriented to time place and person.
No Pallor
No icterus.
No cyanosis.
No lymphadenopathy.
No Clubbing.
No Pedal edema
SYSTEMIC EXAMINATION:
P/A:
INSPECTION:
Abdomen- large, round, no distention, inverted umbilicus.
No scars, sinuses, dilated veins and swellings.
Palpation:
Soft, tenderness present in epigastric region
No signs of organomegally
Percussion:
No fluid thrill, shifting dullness absent
Auscultation:
Bowel sounds heard 2-3/ minute
CVS:
Inspection:
chest- bilaterally symmetrical
Trachea is central.
Apical impulse not seen.
Palpation:
Apex beat felt at 5th ics 2cm lateral to the mid clavicular line
trachea- central
Auscultation:
S1 and S2 heard
no murmurs.
RESPIRATORY SYSTEM:
Bilateral air entry is present
Normal vesicular breath sounds are heard.
CNS EXAMINATION:
No focal neurological deficits.
INVESTIGATIONS:
PROVISIONAL DIAGNOSIS:
RECURRENT ACUTE PANCREATITIS. WITH LICHEN SIMPLEX CHRONICUS.
T/t:
1. NBM
2. IV FLUIDS - 2 UNITS MS, 3 UNITS RL, 2 UNITS DNS @125 ML
3.INJ TRAMADOL 1amp in 100ml NS IV/SOS
4.INJ THIAMINE 1amp in 100ml NS IV/BD
5.INJ ZOFER 4mg IV/SOS
6. SYP LACTULOSE15 ML PO/BD
FOLLOW UP:
11:4:2023:
1. Liquid diet-->soft
2. IV FLUIDS - 1 UNIT NS,
2 UNITS RL, 1 UNIT DNS @125 ML
3. to 6. is the same as previous day
7. Tab LORAZEPAM 2mg PO/OD
8. Tab. BACLOFEN 20MG PO/OD
9. PROSAPALIC NF ointment L/A ODx1 week
10. VENOSIA MAX LOTION L/A BD x4 weeks
FOLLOW UP: 12:4 2022
No complaints of nausea and vomiting
No fever spikes
Pt is conscious , coherent , cooperative
BP-130/80mmHg
PR- 88 bpm
Temp- 96.8F
RR-18 cpm
Input/output-2380/1050ml
GRBS-108mg/dl
CVS- S1,S2 heard, no murmurs
RS- BAE (+), NVBS(+)
P/A- Soft,no tenderness, no organomegally
Bowel sounds present
CNS: NAD
T/t:
1. Plenty of oral fluids
2. soft diet -->normal diet
3. Tab THIAMINE 200 MG PO/BD
4. Tab ULTRACET 1/2 tab PO/SOS
5. SYP LACTULOSE 15 MP PO/HS
6. 8. to 10. same as previous day











Comments
Post a Comment