This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Radhesh Mahankali.
73 year old male came to general medicine OPD with chief complaints of shortness of breath since 2 days
HOPI:
Patient was apparently symptomatic 2 days back then he developed shortness of breath great to which is gradually progressive in nature and progressed to grade 4, no postural and diurnal variation, aggravated on physical activity releived on rest. Patient has scaly plaques on both of his limbsfrom past 7 years for which he used unknown medications.
No chest pain, no orthopnea, no paroxysmal nocturnal dyspnea, no night sweats, no chest tightness, no palpitations, no cough, no fever, no myalgia, no acid reflux, no syncope, no hemoptysis, no decreased urine output, no abdominal distention.
PAST HISTORY:
Had a Leg surgery 10 years ago, malunion is present.
K/c/o TB 10 Years ago for which he was treated(ATT).
N/k/c/o DM, Asthma, HTN, epilepsy, CVD, etc.
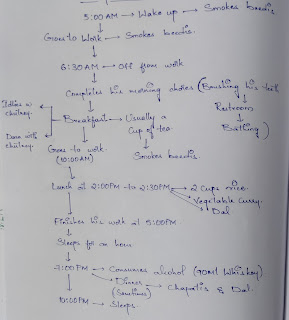
PERSONAL HISTORY:
Diet: mixed.
Appetite: Decreased since 3 days.
Sleep: Adequate
Bladder: Normal
Bowel: Normal
Addictions: Alcoholic since 50 years, Quit 5-6 years ago.
Smoker since 50 years, 1 pack per day.
FAMILY HISTORY:
Not significant.
VITALS:
Temperature: Afebrile.
PR: 75bpm.
RR: 18cpm.
BP: 130/90 mm hg.
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative, well oriented to time place and person.
Pallor present.
No icterus.
No cyanosis.
No lymphadenopathy.
No Clubbing.
Pedal edema present (pitting type) from below the knees.
SYSTEMIC EXAMINATION:
CVS EXAMINATION:
INSPECTION:
Chest wall shape is normal
bilaterally symmetrical
No precordial bulge
No Pectus carinatum/excavatum
No Kyphoscoliosis
No Dilated veins, scars and sinuses
Apical impulse seen at 5th ICS midclavicular line.
No other Pulsations are seen.
JVP( not inspectable due to central line).
PALPATION:
All inspectory findings are confirmed.
No local rise of temperature.
Apical impulse- felt and is normal.
No thrills are felt.
AUSCULTATION:
S1&S2 heard
no murmurs.
RESPIRATORY SYSTEM EXAMINATION:
INSPECTION:
Chest is bilaterally symmetrical
Trachea - midline
No crowding of ribs, Harrisons sulcus
No Kyphoscoliosis, winging of scapula, prominence of the medial border of scapula
No Sinuses, scars, dilated veins and nodules.
PALPATION:
All inspectory findings are confirmed.
Tactile Vocal Fremitus -
Percussion: dull note heard at inframammary area left side
AUSCULTATION:
Decreased breath sounds heard in the left and right inframammary areas.
P/A: SOFT AND NON TENDER.
CNS: NO FOCAL NEUROLOGICAL DEFICITS.
INVESTIGATIONS:
4-04-2023:
5-04-2023:
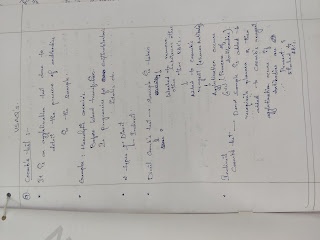
PROVISIONAL DIAGNOSIS:
CKD WITH HEART FAILURE WITH LEFT SIDED PLEURAL EFFUSION UNDER HEMODIALYSIS.














Comments
Post a Comment