This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Radhesh Mahankali.
68 year old female resident of ramannapeta was a labour by occupation came with chief complaints of :
Pain abdomen since 8 days.
Abdominal distension since eight days.
Fever with chills since six days.
Loose stools since six days.
HOPI:
patient was apparently asymptomatic eight days back. Then she developed pain abdomen in the left lumbar region radiating to hypogastric region which was colicky type and was insidious in onset gradually progressive aggravated on food intake, the aggravation is more to solids than liquids.
She then developed abdominal distension since eight days, which was insidious in onset and gradually progressive.
She also developed fever which is intermittent, associated with chills and rigors , no evening rise of temperature, associated with vomitings 3 episodes which are non projectile, bilious in nature, food particles as content.
She developed loose stools 3-4 episodes which lasted for 6 days, watery in consistency, not associated with blood and mucus, black coloured stools.
She visited ramannapet govt hospital for the above complaints where she was admitted for 2 days, there were no relief of symptoms, so, she visited a private hospital in nalgonda and then they came to our hospital as they couldn't afford the expenses in the private hospital.
Patient also has hypopigmentation of lips since 11 years for which she suspected leprosy and visited a leprosy hospital where it was ruled out and was given an unkwnon topical medication, she took the madication for 1 month and then stopped using it.
Patient also has upper back pain since 10 years, sudden in onset after a shoulder injury, on and off, aggravated on lifting weights and relieves on taking rest.
PAST HISTORY:
No similar complaints in the past.
DM-since 10years under Metformin 500mg po od and glimipiride po od-morning before breakfast
sitagliptin500mg po od and rosuvastatin10mg po od-before dinner.
N/K/C/O HTN, asthma, epilepsy, TB, Thyroid disorders.
PERSONAL HISTORY:
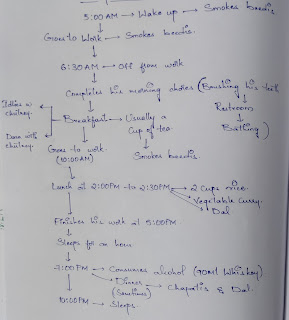
DAILY ROUTINE:
She wakes up at 5 in the morning and she cooks food on her own and drinks juice made of ragi between 7-8 AM
then at 10AM she eats cooked sorghum with curryand has her lunch at 2PM usually rice and curry then she sleeps for an hour and then at 7 pm she has her dinner usually sorghum roti or cooked sorghum with curry and she sleep at 9PM. She was a labour by occupation she quit 5 years ago.
Sleep-disturbed
Appetite- decreased
Addictions- toddy since 20 years, drinks occasionlly 300 ml per session, last cunsumption was 25 days back.
Bowel: loose stools since 6 days
Bladder: regular
Allergies: no known allergies.
GE:
Patient is conscious, coherent, cooperative well oriented to time place and person .Moderately built and moderately nourished
Pallor: absent
Icterus: absent
Cyanosis: absent
Clubbing: absent
Generalized lymphadenopathy: absent
Bilateral pedal edema: absent
VITALS:
PR-70bpm
RR-19cpm
BP-110/70mmHg
temp-Afebrile.
P/A:
INSPECTION:
Shape of abdomen- scaphoid
Umbilicus- inverted
No Scars, Sinuses and engorged veins.
No visible palsations, peristalysis
Palpation:
No local rise of temp
tenderness - mild tenderness in left lumbar region, umbilicus and hypogastric region.
No masses felt Spleen X Liver X
Percussion - No dullness
No Fluid thrill
No Shifting dullness
Aus -Bowel sounds heard.
Cardiovascular System : S1, S2 heard, no
murmurs
Respiratory System : Bilateral air entry present.Normal vesicular breath sounds heard.
Central Nervous System : Higher mental functions intact. No focal neurological deficits.


Comments
Post a Comment